Lung Cancer Surgery Process and Case Studies
Lung Cancer Surgery: Procedure and Key Steps
By Dr. Ching-Yang Wu, Thoracic Surgeon
When a patient is admitted for lung cancer surgery, the entire perioperative process can be divided into four major components, including
(1) Preoperative preparation,
(2) Preoperative surgical simulation,
(3) Preoperative tumor localization, and
(4) Single-port minimally invasive surgery.
Each component plays a crucial role in ensuring surgical safety, accuracy, and optimal postoperative outcomes.
(1)Preoperative Preparation
Before undergoing lung cancer surgery, patients complete several essential evaluations, including
- Biochemical blood tests:
--for nutrition and metabolic status evaluation
--for basic liver and renal function survey
--for basic electrolyte evaluation - Hemogram and coagulation function test
--for Hemoglobin and hematocrits survey (evaluate oxygen delivery Capacity)
--for WBC and differentiate count survey (rule out infection and immunocompromised status)
--for platelet counts survey ( rule out coagulopathy that related to thrombocytopenia) - Echocardiography to assess cardiac function
- Pulmonary function tests (PFTs) to estimate respiratory reserve
- Pulmonary rehabilitation training to improve breathing mechanics
These assessments help determine whether the patient’s general health and cardiopulmonary function are adequate for surgery.
Because lung tissue does not regenerate after resection, surgery is recommended only when the patient’s lung and heart function (ie. cardiopulmonary reserve) can safely tolerate the planned removal of lung tissue.
(2)Preoperative Surgical Simulation
Preoperative simulation is a critical step that enhances surgical precision.
This phase includes detailed review and reconstruction of tumor imaging, allowing the surgeon to plan a safe and accurate operation.
Key components include:
- Evaluating tumor imaging characteristics: Assess the tumor’s shape, density, internal structure, and relationship to surrounding tissue.
- Accurate tumor localization through image reconstruction: High-resolution CT scans are used to map the exact position of the tumor.
- 3D anatomical modeling ( Preoperative simulation):
- Reconstruction of lung anatomy
--visualize the configuration of bronchial and vascular distribution,
--visualized the accurate tumor location ( within specific segment or at junction site between segments)
--Planning the surgical procedure to ensure adequate resection margin with maximal lung tissue preservation
(3)Preoperative Tumor Localization
Small or deep lung tumors may not be easily visible during thoracoscopic surgery.
Therefore, preoperative tumor localization is performed to make lesion visualized and plays an intraoperative marker to make sure accurate resection. Steps include:
- Establishing a reference point on imaging.
- Advancing a fine needle through the chest wall toward the tumor under CT guidance.
- Injecting fluorescent or colored dye near the tumor to create a clearly visible marker.
- Injecting a small amount of contrast to verify that the dye has diffused correctly around the lesion.
In the following example described, the tumor was located in the posterior lung region.
Fluorescent dye allowed precise marking and ensured accurate resection during the operation.
(4)Single-Port Minimally Invasive Surgery
The lung cancer surgery is performed through a single small incision (about 3 cm) using either a thoracoscope or robotic-assisted system.
The major procedural steps include:
- Identify the tumor site and corresponding lung lobe anatomy.
- Carefully dissect and divide pulmonary arteries, veins, and bronchus associated with the targeted lung segment or lobe.
- Inject fluorescent dye from peripheral vascular line and observe under fluorescent scope to delineate the exact boundary between segments ( intersegmental plane)
- Resect the intended lung segment following precise anatomical planes.
This approach minimizes surgical trauma, reduces postoperative pain, and promotes faster recovery.
Case sharing: Steps of Lung Cancer Surgery and Resection Procedure
This case illustrates the complete workflow of lung cancer surgery for a patient diagnosed with a tumor in the left upper lobe.
Through detailed imaging evaluation, 3D anatomical reconstruction, and precise minimally invasive techniques, the surgical team ensured safe and accurate tumor removal while preserving lung function.

The tumor measured approximately 2.4 cc and was predominantly solid in composition.
As shown in Figure B, the solid component accounted for 85.2%, while the ground-glass opacity (GGO) component comprised 14.8%.
Multiplanar CT imaging—including axial, coronal, and sagittal views—further localized the lesion to segments 1 and 2 of the left upper lobe.
Thus, the tumor was characterized as a relatively solid pulmonary nodule with a small volume and a precise anatomical position within the apicoposterior segments.
Following confirmation of the tumor’s characteristics and location, advanced imaging reconstruction software was applied to enhance visualization of the surrounding anatomy.
By selectively removing the pulmonary arterial and venous structures in the 3D model, the tumor’s exact position within the left upper lobe became clear, along with its relationship to the adjacent bronchial branches.
This facilitated detailed preoperative planning and determination of the optimal resection strategy.



In this lung cancer case study, once the pulmonary arteries and veins were reconstructed and visualized (Figure B), the anatomical relationships initially appeared complex.
However, after further refinement of the 3D model and systematic re-labeling of the vascular structures, the tumor’s relative position within the entire left upper lobe became clearly identifiable, as demonstrated in Figure C.

Based on the integrated reconstruction of images A, B, and C, Figure D confirmed that the tumor was situated segment 1/2 of the left upper lobe.

In this lung cancer surgery case, the red region in Figure D represents the ascending pulmonary artery, while the green and black regions denote the segmental bronchi extending toward the tumor.
The intersegmental fissures were relatively well developed, consistent with the findings from the reconstructed imaging.
After confirming these anatomical relationships, preoperative surgical simulation was subsequently performed.
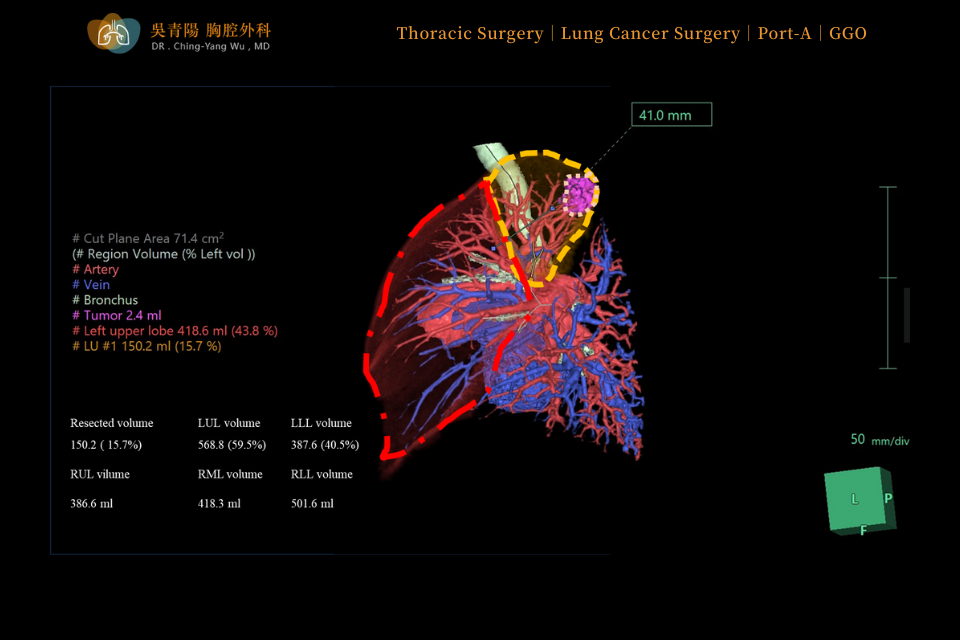
In this lung cancer surgery case, the purplish-red region on the image represents the tumor, the yellow area indicates the planned extent of resection, and the red box outlines the portion of the left upper lobe intended to be preserved postoperatively.
The surgical margin—the distance from the tumor to the resection line—was approximately 4 cm.
The estimated resected lung volume was 150.2 cc, accounting for 15.7% of the left upper lobe and 6% of total lung capacity.
Based on the surgical simulation, the tumor was located within the left upper lobe, and resection was planned for segments 1 and 2, providing a margin of approximately 4.1 cm.
Because the lesion was situated posteriorly, Figure F illustrates that, after establishing a reference point, a fine needle was advanced toward the tumor for CT-guided puncture.
Following successful puncture, fluorescent dye was injected, as shown in Figure G.
To ensure accurate localization, a small amount of contrast was subsequently introduced to confirm that the dye had been placed adjacent to the tumor, thereby completing the localization procedure.
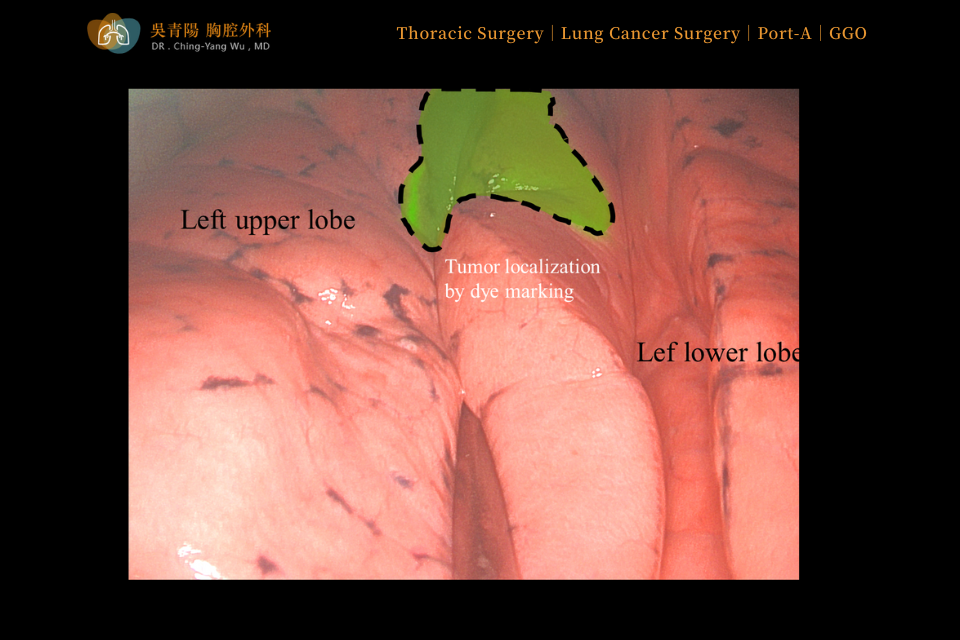
Before the lung cancer surgery began, the stained tumor area was clearly identified in the left upper lobe, where the interlobar fissure was well developed.
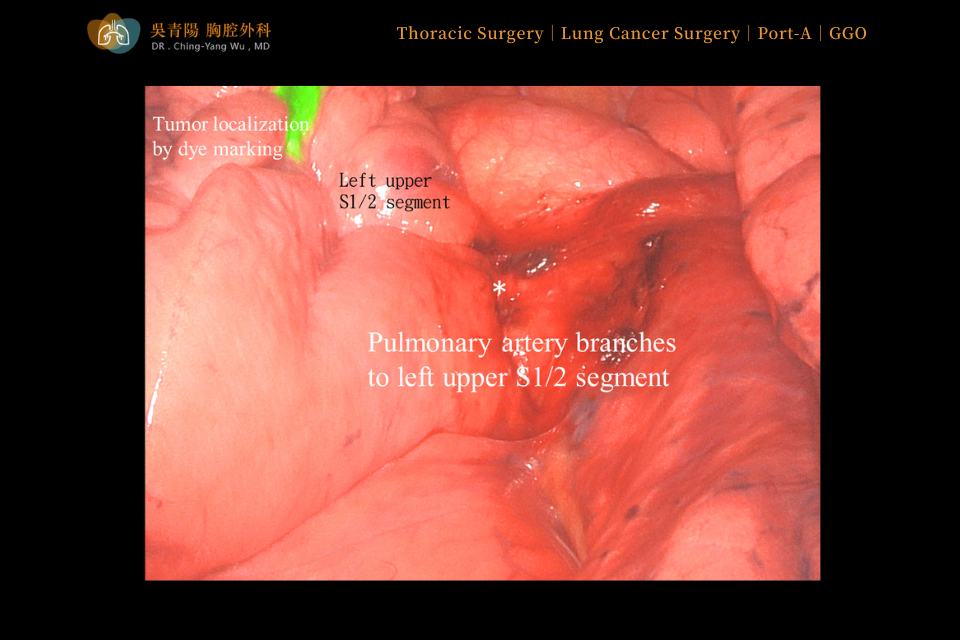
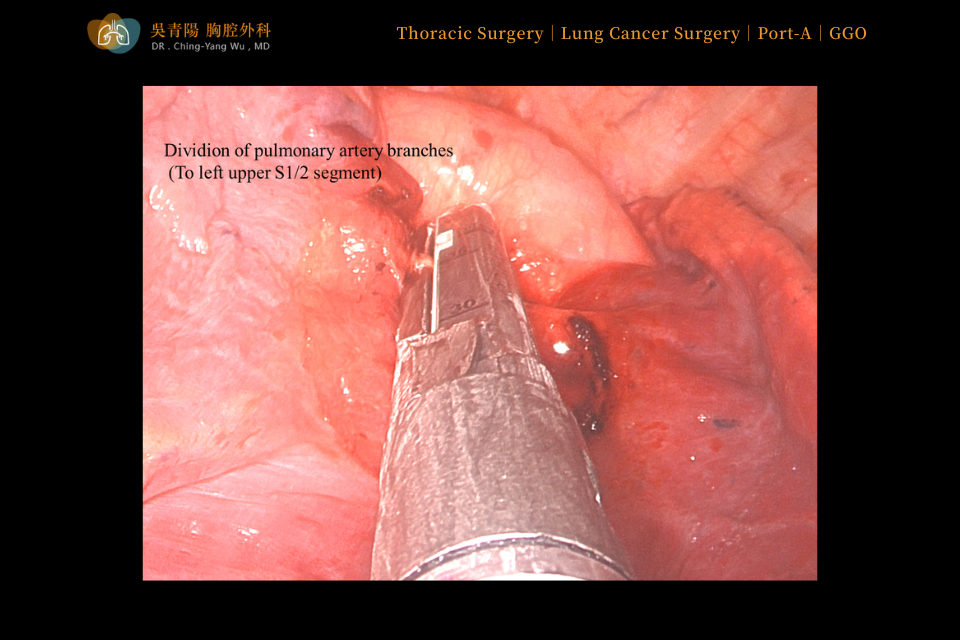
After confirming the tumor location during lung cancer surgery, the fissure between the upper and lower lobes was opened, allowing exposure of the pulmonary artery branches supplying segments 1 and 2 of the left upper lobe.
These arterial branches were carefully dissected, then securely sealed and divided using an endoscopic stapling device.
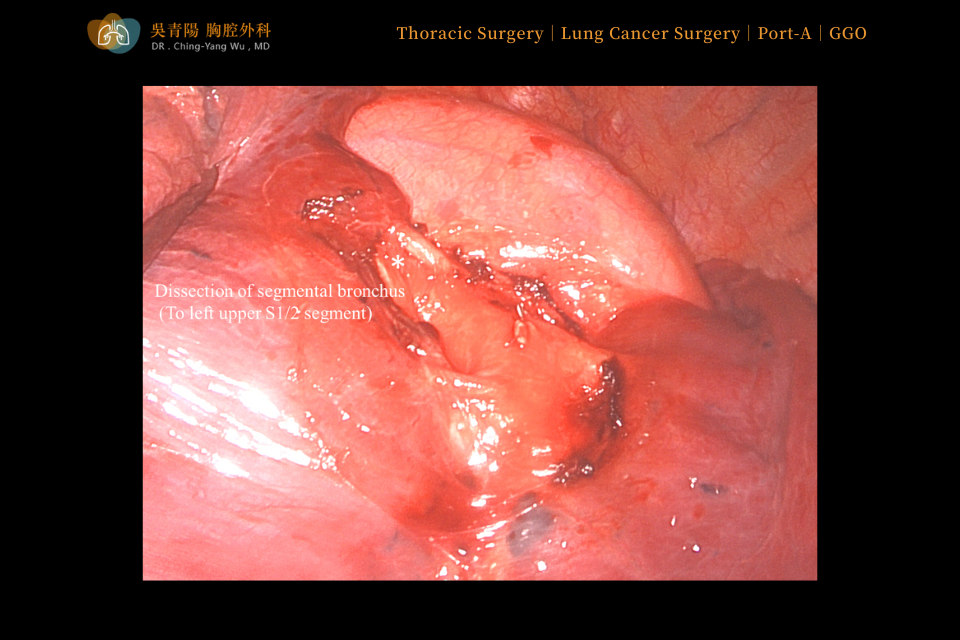
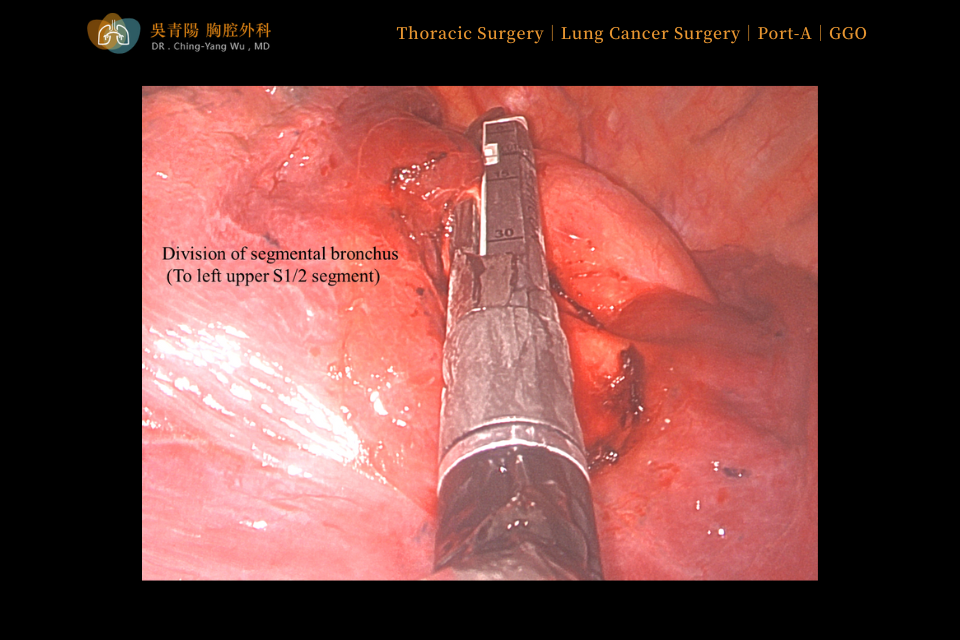
After the corresponding pulmonary artery branches were divided, the bronchi of segments 1 and 2 of the left upper lobe were identified, meticulously isolated, and subsequently sealed and divided.
Following bronchial division, indocyanine green (ICG) was administered through a peripheral intravenous line.
Because the segmental arteries supplying the planned resection area had already been transected, the targeted segments no longer exhibited ICG enhancement, whereas the preserved lung segments fluoresced normally.
With the aid of fluorescence endoscopy, the intersegmental plane was clearly visualized, enabling the surgeon to perform an accurate and anatomically precise segmentectomy along the well-defined boundary.
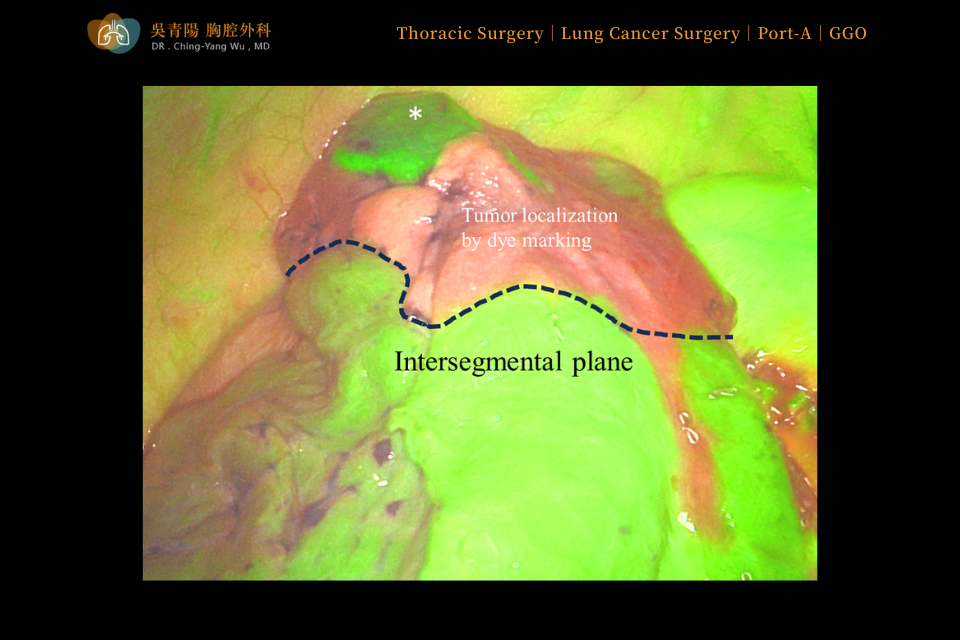
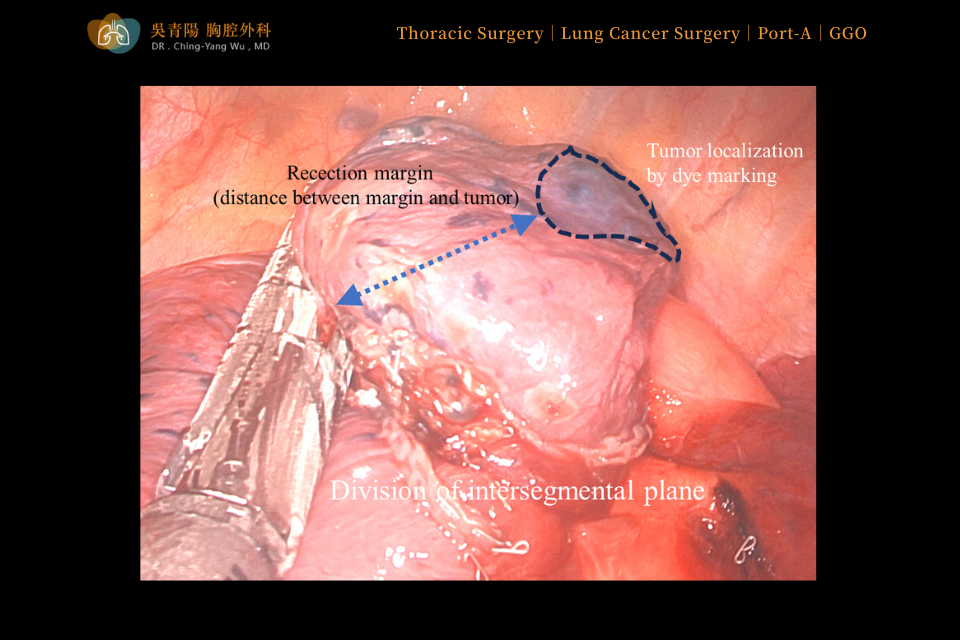
The boundary between the fluorescent and non-fluorescent areas represented the natural anatomical separation of the lung segments.
This confirmed that a safe distance was preserved between the dye-marked tumor site and the planned surgical resection margin.
Once the anatomical boundary was clearly confirmed, the surgeon proceeded with resection of segments 1 and 2 of the left upper lobe using an automatic stapler, following the natural intersegmental plane.
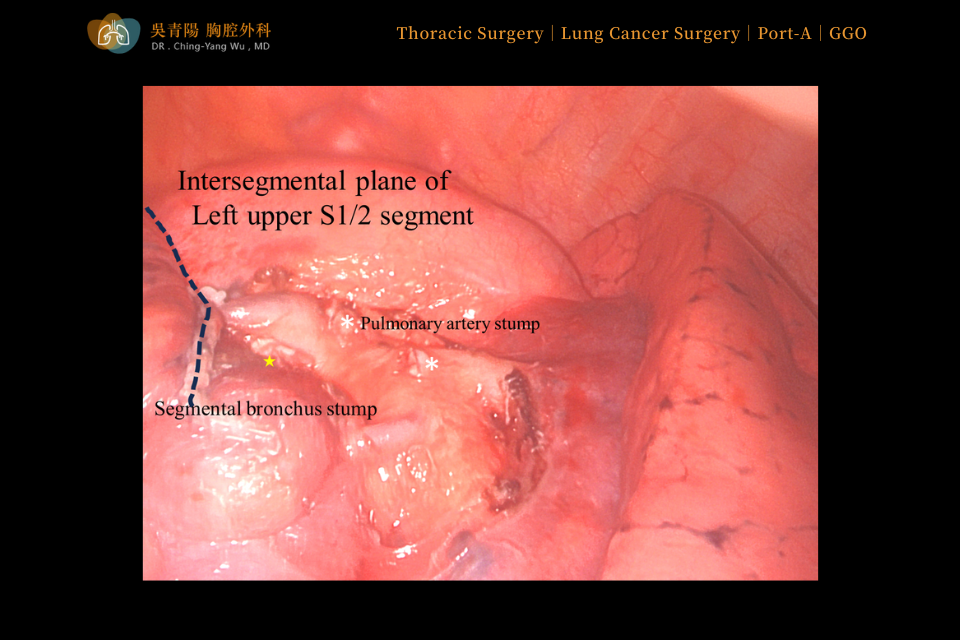
After completion of the resection, the white asterisk marked the pulmonary artery stump, the yellow asterisk indicated the bronchial stump, and the dark blue region represented the junction between segments 1, 2, and 3 of the left upper lobe in this case.

This lung cancer surgery can be performed through a single incision of approximately 3 cm, making it a highly effective minimally invasive procedure.